Will telemedicine be the new norm after the coronavirus crisis?
As the pandemic forces doctors to turn to online solutions, many healthcare providers say they now see their advantages.

When Dr Mythili Krishnamurthy, an obstetrician/gynaecologist in the Indian state of Tamil Nadu, got her patient’s message on WhatsApp about breast pain and a fever, she was confined to her home, like the rest of India, which had been on lockdown since March 25 due to the coronavirus pandemic. But the lockdown did not stop her from managing the patient’s care.
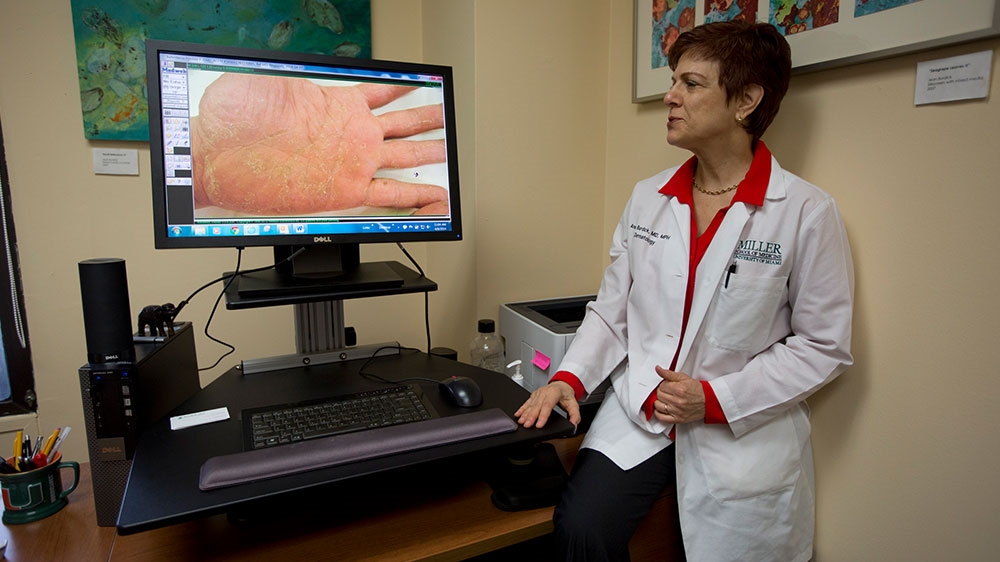
Doctors, like Krishnamurthy, are doing “house calls” again – but now, they are in the form of telemedicine visits. Telemedicine refers to remote care, including real-time video and app-based visits. Because of the public health crisis, a profession wary of accepting telemedicine has turned to it overnight.
Keep reading
list of 4 itemsMexico’s teachers seek relief from pandemic-era spike in school robberies
‘A bad chapter’: Tracing the origins of Ecuador’s rise in gang violence
Why is the US economy so resilient?
Media touts telemedicine’s value as a way to triage suspected COVID-19 patients, but telemedicine is not just a useful temporary stopgap, healthcare professionals say. It allows doctors to see patients with a range of problems and can improve patient care. Once doctors and patients use it, it is unlikely they will stop.

Poor technological infrastructure and low overall computer literacy in Tiruchirappalli, Dr Krishanmurthy’s city, made her look for a simple platform to conduct telemedicine. She chose WhatsApp, a mobile app not specifically intended for healthcare.
“Our health system is low-resource. Few people have insurance coverage. All payments are out of pocket. I could not pass the cost of an electronic medical record or video conferencing to the patient,” she told Al Jazeera. At her hospital, Sri Dhanvanthri Nursing Home, all records are still on paper.
Text communication promoted timely, secure and affordable care.
“Initially, calls were infrequent, but now patients almost all have smartphones so they can talk to me and it saves a lot of time and travel. If they travel 60 or 70 kilometres (47-43 miles) in the night to see me, it makes sense.”
But she acknowledged using WhatsApp and other technologies do come with disadvantages: Texting requires a basic literacy and doctors and patients can also miss nonverbal cues such as facial or physical expressions when they text.
“Using WhatsApp requires an individual rapport between doctor and patient,” said Dr Krishnamurthy.
Until recently, official telemedicine guidelines in India were vague. But on the first day of the lockdown on March 25, the Medical Council of India introduced telemedicine practice guidelines, making WhatsApp an approved platform.
New ‘believers’
Although telemedicine has been available in many countries for years, with some places even setting up telemedicine centres, it did not have wide acceptance in many places. Many patients, especially in rural areas, were not aware it was an option and many patients, physicians, and healthcare systems resisted accepting it as legitimate patient care.
Barriers to implementing telemedicine have included cost, liability, security, lack of technological infrastructure, and poor computer literacy among patients and doctors.
Despite these barriers, telemedicine has its advantages, experts say, as it increases access to primary and specialist medical care. During the COVID-19 pandemic, access to healthcare has decreased because non-urgent in-person visits are discouraged.

Aside from improving access and decreasing patients’ financial and travel burden, telemedicine can also improve care compared with in-person visits.
“I hadn’t realised how much our exam rooms give us a flat view of our patients. Now it’s like being surprised by a pop-up book when I turn on the screen,” said Dr Su Wang, a medical director at Saint Barnabas Medical Center, in New Jersey.
Dr Wang is a recent convert to telemedicine. Because of the COVID-19 pandemic, her clinic switched to mostly online visits out of necessity. Previously, she assumed telemedicine was “subpar” care. She scoffed at video physical exams. But after just one week of telemedicine visits, she is a believer. Real-time video visits gave her a more intimate, and ultimately more comprehensive view of her patients, she said.
“It’s like I’m going into their world for the first time. This is what we miss when doctors stopped doing home visits,” she told Al Jazeera.
She recalled a man she had treated for years. He had always been quiet and shuffled uncomfortably in her office. His family suspected a movement disorder. But on a video visit, the same patient walked easily to his own kitchen to make tea.
Telemedicine also made medication management easier as Dr Wang could peer directly into his medicine cabinet.
“He’s got a pile of meds, and it’s a little disorganised. And I don’t know how he knows which meds he’s taking,” she said, adding that she thought to herself that she hoped he was not taking the medicine she had discontinued.
“Okay this was from two years ago, you must dispose of that,” she told him.
A years-long change in two weeks
Even if three in four Americans are ordered to stay home, doing so should not be at the cost of worsening existing health conditions. “I don’t want to sit on uncontrolled hypertension,” Dr Wang said.
Doctors, including her, assumed seniors would not be technologically savvy enough to use telemedicine. This assumption has not held up, she said of her own patients.
“We just saw four people over the age of 70. And somehow they figured this out. So we should not assume that seniors don’t know how to use their phones.”
In the US, among the biggest barriers to implementing telemedicine have been concerns about reimbursement. Only 10 states required equal payment for telemedicine and in-person visits. The technology required training time and could be expensive. More than other countries, legal issues such as privacy, liability, licensing and security have emerged as additional concerns.
In March, the US’s major governmental healthcare programmes, Medicare and Medicaid, waived many geographical and billing limitations for telemedicine. Private insurers quickly followed.
“We had not really pushed it beforehand, because it was just really not on our mind. If it hadn’t been for this, there would have been so many approvals required from our institution,” Dr Wang said.
The pandemic made a years-long process happen in a few weeks.
“We need to decrease foot traffic. We need to protect the patients, and we need to protect our healthcare workers as much as we can,” she said. With the implementation of telemedicine, Dr Wang’s primary care clinic is humming along – virtually.
She does not see medicine ever going back to where it was before the pandemic.
“I think we’ll end up having better care if we have a mix of virtual and in-person visits. Patients still understand the in-person visit is better, but maybe we don’t need it every single time.”