Coronavirus tests hospitals in parts of US as some states reopen
Coronavirus outbreaks in some areas of the country are straining public health networks.

From a hospital on the edge of the Navajo Nation to the suburbs of the nation’s capital, front-line medical workers in coronavirus hot spots are struggling to keep up with a crushing load of patients while lockdown restrictions are lifting in many other parts of the United States.
Governors are starting to slowly reopen some segments of their local economies, pointing to evidence that the numbers of COVID-19 deaths and new hospitalisations are peaking or starting to recede in their states. But a government whistle-blower warned Thursday that the US faces its “darkest winter in modern history” unless leaders act decisively to prevent a rebound of the virus.
Keep reading
list of 3 itemsUS economy loses a record 20.5 million jobs in April
Study: NYC coronavirus death toll higher than official tally
While many state and local officials see modest signs of progress in the pandemic fight, coronavirus outbreaks are testing public health networks in pockets of the US.
One of those is a suburb of Washington, DC. The head of a hospital system in Maryland’s Prince George’s County, a majority African-American community bordering the nation’s capital, said the area’s intensive care units are “are bursting at the seams”. Meanwhile, a civil rights group’s lawsuit claimed the county’s jail failed to stop an “uncontrolled” coronavirus outbreak and isolated infected prisoners in cells with walls covered in feces, mucus and blood.
“I would say we are the epicentre of the epicenter,” said Dr Joseph Wright, interim CEO of University of Maryland Capital Region Health.
A hospital in Gallup, New Mexico is on the front lines of a grinding outbreak in the Navajo Nation that recently prompted a 10-day lockdown on the city, with police setting up roadblocks to discourage non-emergency shopping.
Medical staff last week staged a street protest to complain of inadequate staffing and urge the CEO of Rehoboth McKinley Christian Health Care Services to resign. The departure last week of the hospital’s lung specialist has limited its ability to treat COVID-19 patients, as people with acute respiratory symptoms are transported to Albuquerque facilities about two hours away. About 17 nurses were cut from the hospital’s workforce in March, at least 32 staff have tested positive for the virus, and the facility’s intensive care unit is at capacity.
“My staff is physically exhausted, emotionally exhausted and they are suffering from moral injury,” said Felicia Adams, the hospital’s chief nursing officer.
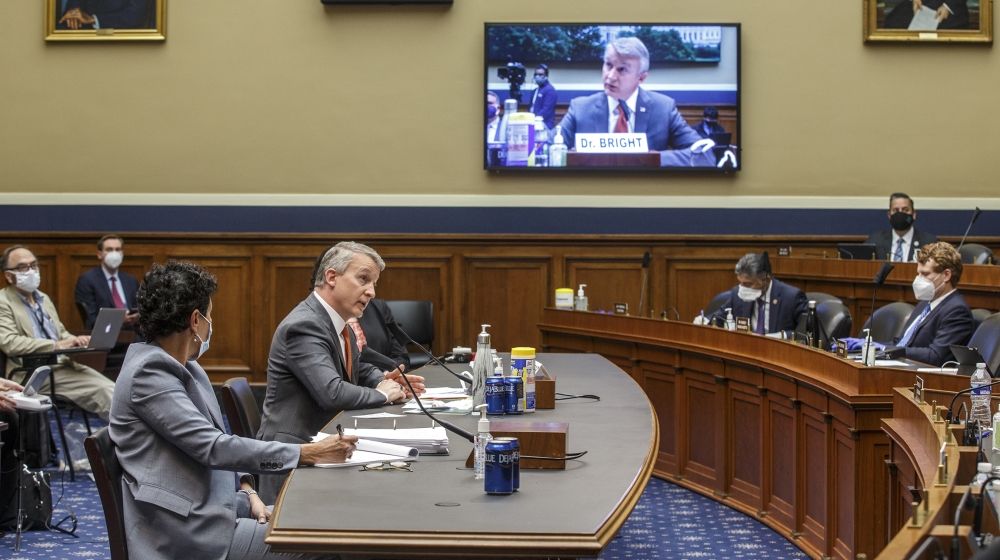
Meanwhile, in Washington, Dr Rick Bright, a vaccine expert who alleges he was ousted from a high-level scientific post after warning the administration of US President Donald Trump to prepare for the pandemic, told a congressional panel that the US lacks a plan to produce and fairly distribute a coronavirus vaccine when it becomes available.
Asked by lawmakers if Congress should be worried, Bright, who wore a protective mask while testifying, responded: “Absolutely.”
Trump on Thursday dismissed Bright in a tweet as “a disgruntled employee”. The White House has launched what it calls “Operation Warp Speed” to quickly produce, distribute and administer a vaccine once it becomes available.
Bright’s testimony follows a warning earlier in the week from Dr Anthony Fauci, the government’s top infectious disease expert, that rushing to lift store-closing and stay-at-home restrictions could “turn back the clock,” and lead to more suffering and death, complicating efforts to get the economy rolling again.
The US has the largest coronavirus outbreak in the world by far: more than 1.4 million infections and nearly 85,000 deaths, according to a tally by Johns Hopkins University. Worldwide, the virus has infected more than 4.4 million people and killed more than 300,000. Experts say the actual numbers are likely far higher.
The pressure is on to staunch job losses in the US after the unemployment rate soared to 14.7 percent in April, the highest since the Great Depression of the 1930s. Another nearly three million laid-off workers applied for US unemployment benefits last week as the viral outbreak led more companies to slash jobs even though most US states have begun to let some businesses reopen under certain restrictions.
Roughly 36 million people have now filed for jobless aid in the US in the two months since the coronavirus first forced millions of businesses to close their doors and shrink their workforces, the US Department of Labor said Thursday.
Many states are lifting lockdowns, leading to tentative resumptions of commerce. But even in those places, hospitals continue to operate on an emergency footing.
In Georgia, the state provided a network of hospitals with extra nurses so its exhausted employees could take some time off and recover. The Northeast Georgia Health System, which operates four hospitals, is still struggling to buy as many disposable protective gowns as it needs. It has assigned workers to collect and sanitise the suits so they can be reused. Community volunteers are sewing gowns and masks.
“That’s our most critical need,” said Tracy Vardeman, the health system’s chief strategy officer. “We’re going through as many as 6,000 a day.”
The system’s largest hospital serves a county at the epicentre of the state’s poultry industry. About one-third of Hall County’s 200,000 residents are Hispanic or Latino, a demographic that has accounted for up to 60 percent of the hospital system’s COVID-19 patients. Officials are taking virus testing to a grocery store in the heart of the Hispanic community.
“I think there is increasing realisation that this is a severe issue and we cannot take it lightly,” said Dr Antonio Rios, a leader of the hospital system’s affiliated physicians’ group.
Wright, the hospital CEO in Prince George’s County, said the three emergency departments that his medical system operates are steadily seeing upward of 70 new COVID-19 confirmed and suspected patients every day. On Wednesday, the emergency departments averaged 3.5 coronavirus patients per hour.
Officials there say the community has been uniquely affected by the virus in part because it is a gateway to the District of Columbia, and many of its 909,000 residents are essential workers who continue to go to jobs every day. That largely mirrors the scenario earlier this spring in Queens, which became the epicentre of New York City’s outbreak.
“We are certainly still very much in a very busy phase of this surge,” Wright said.