Monkey study raises hope for ‘functional’ HIV cure
Surprise discovery of drugs for intestinal disorders suppressing HIV virus in monkeys spawns optimism for treatment.
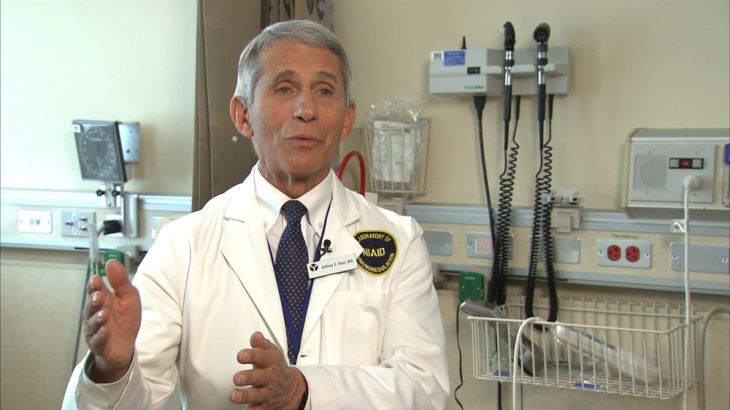
When a drug already taken by thousands of people for intestinal conditions appeared to control the monkey version of HIV, it got Dr Anthony Fauci’s attention.
The director of the US National Institutes of Allergy and Infectious Diseases hopped on a plane to personally tell Japan’s Takeda Pharmaceutical Co’s US representatives their drug may offer a dramatic advance in the fight against AIDS.
Keep reading
list of 4 itemsUS to consider visa restrictions over Uganda anti-gay law
US relaxes restrictions for gay, bisexual men to donate blood
Biden administration appeals US ruling on health coverage mandate
Living with HIV: ‘There is nothing to fear’
Takeda’s drug suppressed the virus to undetectable levels in eight monkeys, some for two years. The findings raise hopes for a so-called “functional cure” – a treatment that puts the disease in sustained remission.
“The data was so dramatic,” said Fauci, who has made AIDS research his life’s work.
|
|
The drug is one of several promising ideas heading into early stage human trials, all seeking to help patients control the virus that causes AIDS for extended periods without daily antiretroviral therapy (ART).
The studies build on research propelled by the case of Timothy Ray Brown, the so-called “Berlin patient,” whose HIV was eradicated through an elaborate stem cell transplant in 2007.
“There has been this explosion of discovery,” said Mitchell Warren, executive director of the AIDS Vaccine Advocacy Coalition. “There are completely new ideas that were impossible to conceive even a few years ago.”
HIV once meant certain death. But, for more than half of the 36.7 million HIV patients around the world, antiretroviral drugs transformed it into a chronic disease.
Taken daily, ART suppresses the virus. But keeping up a daily medication regimen is difficult. The drugs are expensive and toxic, causing nausea, fatigue, and nerve problems in the short-term, and insulin resistance and other problems over time.
Fauci’s visit was a first for Takeda, a company focused on treatments for cancer, gastroenterology, and the central nervous system, said Dr Michael Shetzline, who heads clinical science for Takeda in Cambridge, Massachusetts.
“The excitement was just clear,” Shetzline said. “It was like, ‘Wow.'”
Takeda does not study HIV. But its researchers understood the basic science surrounding its drug Entyvio, an antibody engineered to attack a specific protein.
![Dr Anthony Fauci, director of the National Institutes of Allergy and Infectious Diseases [Gershon Peaks/Reuters]](/wp-content/uploads/2016/12/e06f175f6af541309cea49eb55d36e23_18.jpeg)
The drug, known generically as vedolizumab, is approved in more than 50 countries for ulcerative colitis and Crohn’s disease, which occur when the immune system attacks the intestines.
“Entyvio is a cell trafficking molecule that affects immune responses,” Shetzline said. “In this instance, the GI tract is what is harboring this HIV cell population that needs to be cleared – at least that is what the monkey study implies.”
Takeda is providing the drug and supporting the study. Shetzline cautioned that it’s only a pilot.
“We’d love to see this benefit patients,” he said.
If it pans out, cost could be an issue. Entyvio is priced from $2,000 to $5,000 a month.
Entyvio’s HIV trial began in August and seeks to enroll 15 to 25 people with stable disease. They will remain on daily antiretroviral drugs while taking nine infusions of Entyvio over a period of several months. Then, ART will be stopped, they will get two more infusions, and doctors will watch to see if the virus rebounds – or remains suppressed.
Homeless HIV patient removed for Durban AIDS summit
Manni Baez, 30, of Columbus, Ohio, travels to the National Institutes of Health in Bethesda, Maryland about once a month for the study.
“For me, the end game is providing the folks at NIH with the resources they need to get them closer to finding a cure or a vaccine for this plague,” Baez said.
Fauci said he doesn’t expect meaningful results until late 2017 or early 2018. Even partial success would be huge, he said.
“If we discontinue therapy in the 15, and four of them don’t rebound,” he said, then “that is the best anybody has ever seen.”
|
|