‘Worse than war’: Health workers on a year of the pandemic
A year into the pandemic, front-line health workers around the world share their experience battling the coronavirus.

In the year since the World Health Organization (WHO) declared the coronavirus outbreak a global pandemic, doctors, nurses and medical staff have been at the forefront of the battle against COVID-19.
Front-line health workers around the world have faced enormous challenges to deliver essential care to patients, struggling with a lack of equipment, the constant fear of spreading the virus, and other issues such as social misconceptions relating to their work.
Keep reading
list of 4 itemsMexico’s teachers seek relief from pandemic-era spike in school robberies
‘A bad chapter’: Tracing the origins of Ecuador’s rise in gang violence
Why is the US economy so resilient?
Often isolated, they have seen colleagues and patients die. According to Amnesty International, at least 17,000 health workers have died from COVID-19 over the last year.
New variants of the virus discovered in recent months led to a resurgence of infections. But with some countries rolling out vaccines, and health workers among the first in line to receive shots, there is some sense of hope.
Health workers around the world spoke to Al Jazeera about their experiences over the past year and their hopes and fears for the future. Below are their stories.
Dra Anne Menezes, Brazil
When Dra Anne Menezes arrives to work at the emergency COVID-19 ward at Getulio Vargas Hospital, Manaus, she has to decide which patients to stabilise and which require intubation. The city in Amazonas state is the epicentre of the outbreak in the country, where a second wave of the virus is becoming more vicious.

“We’re extremely exhausted. We’ve been battling this virus for a year now. We deal with death every day and it’s affecting us all psychologically. When the health system collapsed in January, there was also a collapse in healthcare professionals. We lost a lot of family members and colleagues. We arrived at the hospital afraid, there was a lot of insecurity.
“What is really worrying is that compared to the peak of infections last year, patients in their 30s to 50s are now developing severe symptoms. For example, we lost a young otologist colleague due to COVID complications, as well as a 44-year-old patient. We fought to keep the patient alive, it was like a warzone.
“It’s shocking that people here don’t respect social distancing measures or wear masks. Since the government reopened the economy, people have returned to crowded parties. We’re now waiting for the third wave to hit. Despite all of this pressure, the company of my colleagues has lightened the mood. We give support to the other so that we don’t fall. Otherwise, we couldn’t keep going.”
– Reporting by Charlotte Peet.
Dr Jehad al-Ja’idi, Gaza
Dr Jehad al-Ja’idi is the director of the intensive care department at the European Hospital in the besieged Gaza Strip. It is the main site in Gaza for patients with severe and moderate cases of COVID-19.

“In the last 20 years that I have worked in Gaza hospitals, I faced a lot of difficult situations, but COVID-19 is worse than wars. In a war, the wounded cases come anaesthetised, or they can be anaesthetised, but with coronavirus, you see the patient in front of you losing the ability to breathe. Sometimes after you have dealt with the patient for several weeks, you may lose him suddenly regardless of his age.
“My staff and I expect to be infected any day. It is hard for our families, as we try to go back home but we avoid kissing or hugging our children, and we keep our selves isolated. Twenty percent of my staff was infected with COVID-19 while treating patients.
“The biggest challenge we faced is the shortage of PPE, and noninvasive ventilation equipment. We have limited items in the ministry storage to face this virus. The Gaza context is difficult, due to the dependency on international aid amid the Israeli siege. But there was an advantage due to the restrictions on travel – this delayed the arrival of COVID-19 compared to other countries and gave us time to prepare our hospitals to receive the first cases.”
– Reporting by Hana Salah.
Dr Manggala Pasca Wardhana, Indonesia
Dr Manggala Pasca Wardhana, 36, is an obstetrician-gynaecologist at Dr Soetomo Hospital in Indonesia’s second-largest city of Surabaya.

“In obstetrics and gynaecology, the impact has been quite extraordinary. Imagine that as of March 2, 325 doctors have died in Indonesia, and 20 of them were obstetrician-gynaecologists, making the proportion the second-highest after general practitioners. For childbirths, however, there could not be any delay and everyone came with conditions that needed to be taken care of immediately. Most deliveries [of patients] with COVID-19 were asymptomatic, so it was impossible for us to differentiate whether these patients had COVID-19 or not simply from interviews and regular examinations.
“I myself am a COVID-19 survivor. I contracted it while doing a Caesarean section in a case of pregnancy with a complex problem – placenta accreta which was very risky to heavy bleeding – and unfortunately, this patient was also exposed to COVID-19. The operation went well, the mother and baby survived, but unfortunately, most of the members of the operation ended up testing positive for COVID-19.
“During this pandemic, working at the hospital every day is clearly worrying. [My] family is also very worried. At home, I use one room to self-isolate until I am absolutely sure that I am not infected, and I do this periodically every time I have exposure [to the virus] or I feel unwell. What worried me first is, of course, not myself, but my family. I am really scared this could infect my family.”
– Reporting by Randy Mulyanto.
Junior Doctor Ithra Ganijee, South Africa
Junior Doctor Ithra Ganijee was in the first year of her medical career when the pandemic hit. As South Africa’s first wave took hold, she was among the staff on the COVID-19 ward at New Somerset Hospital in Cape Town.

“There were so many moments where I felt so overwhelmed and overworked, particularly as colleagues began contracting the virus meaning that often we would be covering for others while also carrying out our own duties. It was the support from senior members of staff was that really helped me to adapt quickly to the constantly changing circumstances.
“As the first wave went on, I too got COVID-19, and while my symptoms were mild, having to isolate was incredibly difficult. A few months on the numbers began to settle and there was this feeling of calm. Soon we began to see cases rise and towards the end of 2020 the second wave arrived. Though this time the hospital was better prepared, there is no denying that the healthcare system across the country was under immense strain and by extension so were front-line healthcare workers.
“Above all, the rollout of the vaccine has provided us with something we’ve been without for a while; hope, in what has been a dread-filled year. Many health workers I know have been inoculated and this feels like such an achievement, now we are keeping our fingers crossed that things go to plan, meaning that relief is in sight.”
– Reporting by Samira Sawlani.
Dr Maurocrop Daguino Ayala, Bolivia
When Dr Maurocrop Daguino Ayala arrives at the coronavirus emergency room in Municipal Plan Hospital 300, one of the main COVID-19 hospitals in Santa Cruz, he not only has to deal with critical patients but has to do so with limited medical supplies.

“During the second wave, it was very different from the first as what we saw was that people of different ages were being more affected, specifically younger people. The fact that young people have continued to go out and bring the virus to their family homes has created a sense of despair. I would not say that the situation is more stable now than it was a few weeks ago when many of the hospitals in my city collapsed.
“In my clinic, we have had to make do with little biosafety equipment. Bolivians are very creative people so we have been using facial masks made from different materials which are either bought or manufactured, but we are still undisciplined with anti-coronavirus measures.
“My working day has changed a great deal during the pandemic, as we have to be more attentive in what we are diagnosing and obviously at this moment we are always looking out for suspect COVID-19 symptoms. Psychologically it’s been hard. Every day, when I get home exhausted, I log onto Facebook praying that I do not encounter a colleague who has died from the virus or a family holding their breath while their loved ones are in the intensive care units.”
– Reporting by Charlotte Peet.
Nurse Victoria Neville, United Kingdom
Victoria Neville, 34, is an intensive care nurse at a hospital in Cheshire, northern England. Neville says that front-line staff at the hospital are struggling to cope with the trauma of the past year and suffering from burnout.

“The second wave has been a lot worse. We have found that the patients are a lot younger and the outcomes aren’t as good. The average age [of patients] on the unit now is between 45-55. During the first wave, it was about 70, and we had maybe 150 patients in the hospital, at a maximum. The maximum this time around is nearly double that.
“Staff are physically and mentally drained. They are off sick with burnout and are using counselling services because it’s a repetitive trauma [working on the front line]. Every shift you go in, there’s a traumatic event. Every shift, there’s a death that you can’t explain in normal terms. On a daily basis, I have to say sorry to multiple relatives for something that actually is out of my control. That has a constant impact on you.
“Looking back, it has been the worst year of my life; I’m exhausted. It has made me consider whether I want to be a nurse, and think about whether I am good enough, at times, to do this. It has just been relentless, and it has taken its toll on even the strongest of people.”
– Reporting by David Child.
Dr Muhaymin Abdel Reda, Iraq
Dr Muhaymin Abdel Reda works in the emergency department of Baghdad’s Shaikh Zayed Hospital.

“Initially, the situation in Iraq was not so bad. But by May or June, the symptoms were a lot more severe, and the number of patients shot up. The worst period was the summertime up until September. We tried to protect ourselves by making sure all hospital staff, including security guards, had PPE. But as the numbers increased, we weren’t able to cope.
“One by one, doctors and nurses fell ill with the virus. I was one of them. I quarantined at home and treated myself with painkillers to cope with the fever and pain. After about two weeks, I was able to return to work. I continued to feel weak for about a month, but I had to help others.
“During the peak weeks of the infection, we, as doctors, had no time to rest. Each of us was trying to help everyone that they could. Many of us isolated from our families to keep them safe as we worked around the clock. Although many people refused to believe that the virus was a real threat and many did not follow safety precautions, we still managed to overcome the worst of the coronavirus in Iraq. It has been an overall successful experience and things have nearly returned to normal here.”
– Reporting by Abdallah al-Salam.
Dr Rahim Khan Babar, Pakistan
Dr Rahim Khan Babar, 29, is a resident doctor at Quetta’s Civil Hospital, the largest government-run hospital in the city and one of the few places in the province of Balochistan that is equipped to deal with serious coronavirus cases.

“The biggest issue here [in the beginning] was that there was propaganda that we would take patients who were sick away and then infect them with poison to give them the coronavirus. There have been attacks on us in the wards, and doctors have been treated like criminals.
“The second issue was that our lives with our families were really badly affected. Most doctors stopped going home, we stayed here at the hospital or the hostels all day. We slept in our ward duty rooms, or we would sleep together huddled in the apartments of other doctors. We knew that we would have been exposed together. I myself spent two and a half months sleeping away from home.
“We faced the maximum level of exposure – I would say more than 70 percent of the doctors here at my hospital tested coronavirus positive at some point. People who were infectious were forced to come to work in the wards wearing masks, because if they didn’t then there wouldn’t be any doctors left. There were very limited resources here [in the first few months] – there was a time when we didn’t have sanitiser, didn’t have masks. But we still worked through it.”
– Reporting by Asad Hashim.
Nurse, DR Congo
She has been in the profession for 14 years and is currently posted at a busy hospital in the Congolese capital, Kinshasa. She requested anonymity citing fears for her safety over stigma related to the coronavirus in the Democratic Republic of the Congo.

“When the country started recording cases what we saw was that a lot of people did not believe COVID-19 existed. This took some time to change and still now there are people that don’t believe it is real. Also while COVID-19 is big, we still have other diseases in the country which are far more common such as malaria. These kinds of illnesses did not just disappear and we also have to continue providing treatment for this.
“One difficult thing which is why I prefer to be anonymous is the stigma faced by some health workers because there are people who think that medical staff will be spreading the infection everywhere we go and so they avoid us.
“I am eager for the vaccine, however, it is now important to educate people about it because already I have met many people who say they will not take it because they are scared. This is largely down to misinformation spreading all over social media. As a healthcare worker having people trust you and the system is an important thing, we have seen the importance of building trust, educating and communicating with communities particularly through COVID-19 and the Ebola outbreaks in this country and the continent.”
– Reporting by Samira Sawlani.
Dr Vojtech Weiss, Czech Republic
Cardiologist Vojtech Weiss has been tending to COVID-19 patients at Prague’s Na Homolce Hospital since October 2020. Weiss explained that all 12 beds in his ward have been full with patients since mid-February, as the country’s infection rate soared to the world’s highest.

“As soon as one bed becomes free, new people are brought in. I feel for our nurses who do the hardest work. The hospital told them they would be able to go back to their work at the gynaecology ward at the start of this year. But obviously, the situation has changed and I can see they are tired and disappointed. One of them even quit because she could not take it any more.
“There is also a lack of information going to the public: the fact that the government puts restrictions in place and proceeds to change them a day later is undermining the severity of the pandemic. I see many COVID patients but also my friends worry about their symptoms at times when the course of their illness is still under control. Many don’t understand at which stage they should seek medical help and what is still treatable at home. It seems like basic information is missing.
“I am also surprised at the lack of cooperation between hospitals. The Czech Republic has a public health care system, so I would expect hospitals to transfer patients when they reach their limits, but this type of communication is lacking.”
– Reporting by Anna Koslerova.
Dr Luis Omar Monarrez Luna, Mexico
Every day starts and ends in “the COVID room” for Luis Omar Monarrez Luna, 39, a doctor from the Mexican border city of Ciudad Juarez.

“The dynamic at home needed to completely change. When I come back home we have to do all the measures first. I can’t come home from work and embrace the kids, I have to go to the COVID room, remove my clothes, put them in a special container, take a shower and then after the entire ritual is complete, I can give hugs and kisses to our kids.”
“My speciality is rehabilitation medicine but all the specialists in the hospital have been converted into COVID doctors. I deal with emergency patients, supporting the emergency units to receive patients and give them the initial protocol treatment. There were moments when the emergency room was full and patients were still arriving. I had to deal with the relatives and explain to them that we can’t accept their relatives even though they needed it, on the verge of death. I knew that whatever explanation was going to be insufficient.
“As a medical professional, I can never show my fear or my sadness, but I felt a sense of impotence over how COVID is being managed in my country. I had to remain calm in order to handle the situation because people depend on this. But during these situations, I had fear and nervousness but I think the training that I have as a doctor would push us forward and give us this calmness, up to a certain degree.”
– Reporting by Jihan Abdalla.
Priyakant Sharma, India
Priyakant Sharma, 37, is a nursing officer at New Delhi’s Lok Nayak Jai Prakash Narayan (LNJP) Hospital and a vaccine supervisor. As the pandemic worsened last year, he sent his wife and children to the family home in Rajasthan, some 320km (200 miles) from the national capital, and stayed behind.

“In the initial months, I felt very lonely. As soon as I would enter my colony [after work], people started running inside their homes. They shut their doors as if I was committing a crime by going to hospital and performing my duties as a front-line health worker. That was heartbreaking but I understand why they did so and soon I started staying away from everyone, I wouldn’t talk to anyone. But with time, they started respecting me for what I do.
“After six months, I couldn’t stay away from my family. I took a test and it was negative and I went home to see them. When I returned to New Delhi I got tested and it was positive. When my father got infected and was admitted to an ICU, it was the most painful moment for me. I felt guilty for his condition until he fully recovered.
“We can say that the situation is under control now. We have got vaccines now which is a good thing and I hope soon this disease is over and we will get back to normal.”
– Reporting by Bilal Kuchay.
Dr Haydar Can Dokuyan, Turkey
Dr Haydar Can Dokuyan works at Dr Nafiz Korez Sincan State Hospital in Ankara. He is also on the board of the Ankara Medical Chamber.
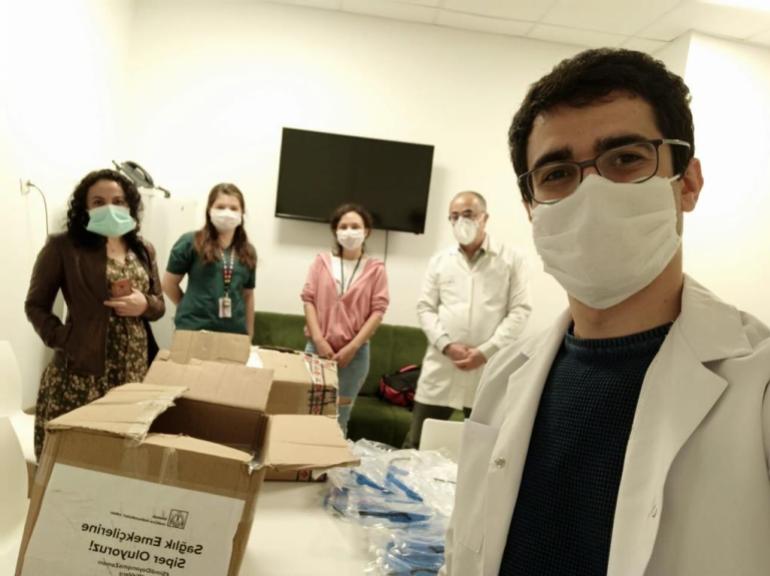
“Even before the pandemic, Turkey’s health workers were working with extraordinary intensity. Most physicians couldn’t spare enough time for their patients. Since the pandemic couldn’t be controlled, unfortunately, non-pandemic health services were disrupted. On the other hand, working in the pandemic wears all of us out. Many are experiencing burnout with the constant worry about getting sick and infecting their relatives.
“During the pandemic, physicians were financially supported with additional payments. However, there were huge inequalities in these additional payments and others, such as assistant physicians, cleaning staff and nurses, didn’t benefit from these additional payments. Overall, I don’t think medical staff are sufficiently supported.
“Since the start of the pandemic, there has been no transparency and, despite calls from Turkish Medical Association [TTB], the actual number of cases wasn’t fully disclosed, which pushed people to complacency. Meanwhile, the TTB and medical chambers were accused of being traitors. Our professional organisation, whose constitutional duty is to protect public health, wanted the epidemic to be managed scientifically and transparently from the very beginning.”
– Reporting by Andy Wilks.