Connecting clues, doctors treat COVID-linked illness in children
Otherwise healthy young patients are falling seriously ill with largely unknown PMIS, which seems to follow COVID-19.
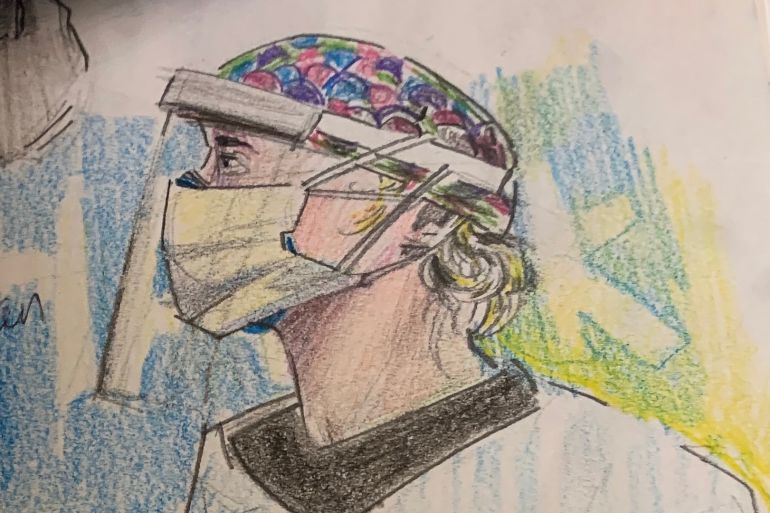
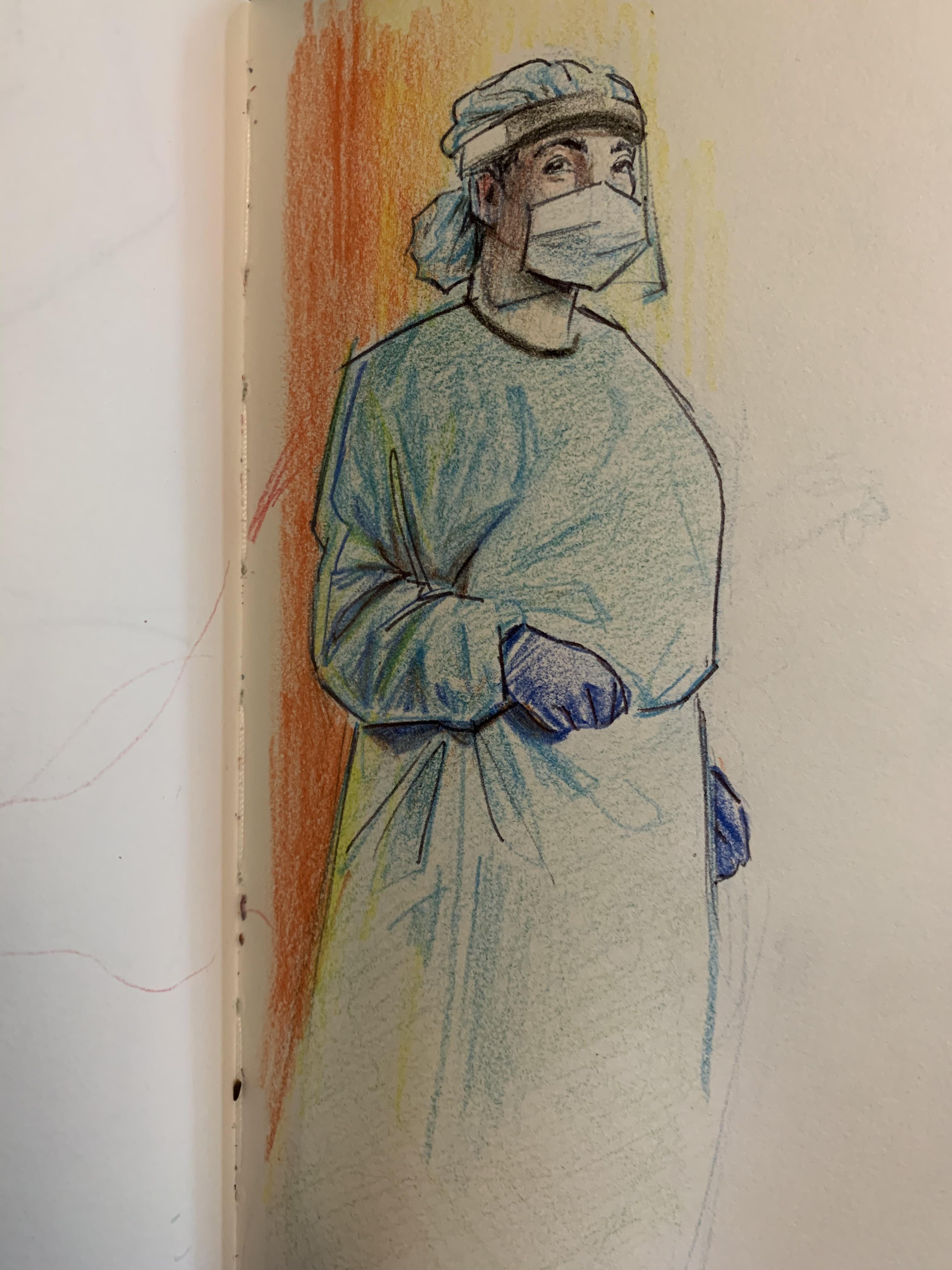
David Vargas loves to draw fellow New Yorkers.
He lives in the Bronx, and uses public transport to visit parks in Brooklyn and Manhattan. He draws people on the subway, and gets lost in the details, like their shoes.
Keep reading
list of 4 itemsMexico’s teachers seek relief from pandemic-era spike in school robberies
‘A bad chapter’: Tracing the origins of Ecuador’s rise in gang violence
Why is the US economy so resilient?
New Yorkers who ride the subway wear so many different shoes, they hold their feet in so many different positions, and sketching shoes is far less awkward than staring a stranger in the face as the train rolls from station to station.
Does he ever miss a stop in order to finish a portrait? Vargas reflects, but then quickly starts laughing, “yes, all the time”, he says.
When Vargas got the coronavirus, the illness was swift and mild. He is 17, and thought nothing of it. A few days later, he felt terrible.
“I’ve never felt anything like it,” he says.
In the evenings, pain started in his chest, but he could not say whether it was coming from his skin, his bones, or his heart. “I didn’t know what was happening to me.” After keeping quiet about it for two days, he told his parents, who took him to the emergency room.
Vargas was one of the first young New Yorkers to experience a rare new illness that appears in children weeks after COVID-19 cases peak in the vicinity, which doctors are calling paediatric multisystem inflammatory syndrome, or PMIS (but other variations of the name include MIS-C, or simply MIS).
The condition – which affects children, from toddlers to teenagers – is defined by a serious inflammatory syndrome affecting multiple organs, and a proven connection between the patient and the virus that causes COVID-19: SARS-CoV-2.
But PMIS is not COVID-19 – it is something that seems to follow it.
A clue in the dark
In New York, where almost 400,000 people have been infected by the coronavirus, just more than 200 PMIS cases have been observed since late April. Scientists are beginning to understand its features and search for its causes.
At first, Vargas did not know what he had, but after spending one night at a local hospital, he was moved to Mount Sinai Kravis Children’s Hospital in Manhattan.
Dr George Ofori-Amanfo, a cardiologist and intensive care physician, leads the paediatric ICU at Mount Sinai. When PMIS children began arriving, he and his team set two goals: treat them, and understand what they were suffering from. In the beginning, all they knew was that the cases were serious.
“It’s an exaggerated, uncontrolled immune response to COVID exposure. By that definition, it could affect any organ of the body, including the heart,” Dr Ofori-Amanfo says.

Vargas would stay at Mount Sinai for a week, spending much of that in the ICU.
“To find out I had a cardiac issue was … very scary,” he says. Each day he met a new nurse or doctor. “Every six hours, they would take a blood test … to measure the level of a specific protein in my blood,” Vargas recalls.
Of particular interest were interleukins, proteins that modulate immune responses within and between cells. Certain interleukins were elevated in these children: it was a clue in the dark.
Dr Ofori-Amanfo watched his patients’ charts in real time. While tracking Vargas’s recovery, the scientists around him were building “a pool of data to [use for] the statistical analysis, and to see the trends,” Dr Ofori-Amanfo explains.
Meanwhile, Vargas rested, talked with the doctors and his family, and drew pictures. “For the first few days … I had a general understanding of what was happening to me, but I got the sense that not even the doctors knew what was happening.”
Dr Ofori-Amanfo hoped to answer a more vexing question about the children in his ICU, some of whom were very sick. “Why does Patient A get this syndrome, and Patient B does not? How can we understand that phenomenon?”

Solving the mystery
In a lab 20 minutes drive downtown, scientists are following two paths to pursue this mystery.
Some patients who have recovered from PMIS are enrolled in a study that aims to identify rare gene mutations that may amplify the syndrome. They look for unique genes shared by the most sick, hoping to illuminate the biological pathways that PMIS – and even COVID-19 – exploits.
The New York Genome Center is the first stop for samples from Dr Ofori-Amanfo’s patients and others who have volunteered to be anonymously analysed. The centre rapidly translates the protein-coding parts of a patient’s DNA and writes the data onto an encrypted hard drive, about 150 gigabytes per patient, which is delivered to the St Giles Laboratory at Rockefeller University, near the Hudson River. Scientists immediately dive into the load: millions of letters of more than 20,000 human genes.
“Everyone is working around the clock. I can’t stress enough, we couldn’t be doing things faster,” said Dominick Papandrea, who manages the volunteers and the incoming samples.
The data is analysed on two tracks. In the first – called the “dry lab” – software compares whole genomes between patients, and spotlights rare gene mutations that appear across multiple people. These candidate genes are flagged, indicating targets for further research.
The dry lab is “unbiased”, ploughing into the raw data without any expectations for what it is looking for. It is also a relatively recent tool in the history of medicine; made possible by the dual breakthroughs of faster computer processing and the capability to work through an entire genome at once.
In 2020, the time between blood withdrawal and data processing is only a few weeks, a speed only imagined 20 years ago. Once the lab receives the data, preliminary findings could come within days.
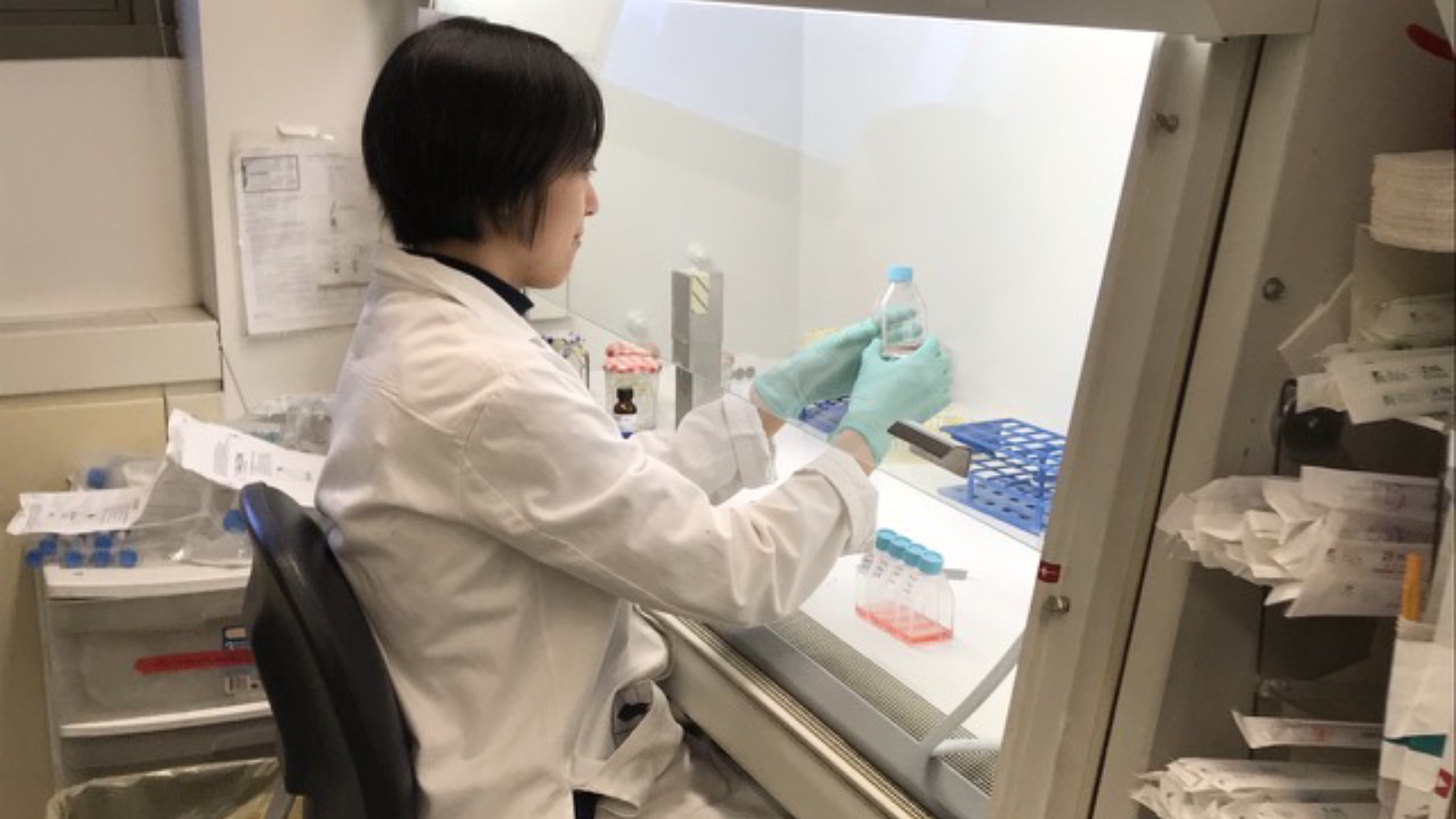
The “wet lab” is where the scientific process unfurls. Here, researcher Dr Qian Zhang begins with a hypothesis about the biochemical pathways most likely implicated in PMIS (and extreme COVID-19). Using the patient’s cells as her toolbox, she prods for weaknesses that begin at a single misspelled gene, testing up the ladder through poorly functioning proteins and missing cells. She can analyse the blood, the immune cells or other pathways. She can induce stem cells to become tissues that were not donated, like neurons or lung cells, and submit them to further scrutiny.
For PMIS, she is beginning with the blood, suspecting that some answers will be hiding there. PMIS shows its most dangerous effects near the heart muscle and in organs critical to the circulatory system. If her colleagues across the partition identify a signal from an unexpected gene, they flag it to her, and she investigates the pathway.
“It’s very difficult to predict how long it takes [to reach results],” Dr Zhang says. “For the severe infection [of COVID-19] we have already seen very promising [gene] candidates, [and] we started in January. For PMIS, it’s just started to come in and my prediction is it will take a couple of months before we can really start to see the mutations that we are confident in.”
A faulty gene?
Dr Jean-Laurent Casanova coordinates this global search. He runs this laboratory in New York, a similar lab at the Institute Imagine in Paris, and since February has built a network that includes dozens of centres on six continents called the COVID Human Genetic Effort.
“There are two lines of research that have converged in recent weeks,” he told Al Jazeera last month. Dr Casanova has tried to find genetic causes behind Kawasaki Disease, the syndrome PMIS is closest to, but after searching for more than 10 years, answers remain elusive.
With coronavirus, he has one viral culprit to tie everything back to.
The human body maintains an arsenal of defences against constant bombardment by foreign infectious agents, like viruses and bacteria. But if a faulty gene for building one component (a protein) is inherited from one or both parents (with misspellings or misplacement of genetic letters), those patients will become sicker than normal patients.
Dr Casanova’s work aims to pinpoint these unique cases, to connect “one gene, one infection” where possible, and discover interventions to supplement missing pieces. Over 25 years of work, Dr Casanova and his team have identified genes that cause a minority of people infected by tuberculosis to become seriously ill, discoveries that led to novel interventions. Now, everyone is focused on COVID-19.
“You don’t need many patients to do genetics. It’s a misconception. You need many patients to do biometrics, [to find] a signal in the midst of a background. But that’s not genetics. For genetics, one patient is enough,” Dr Casanova explains.
Computation is so powerful in 2020 that a thorough look at one person’s genome could alert scientists to a unique faulty biochemical pathway and suggest a repair. This clue could reveal a target against the disease process itself. More than 300 so-called “primary immunodeficiencies” have been identified, genetic errors leading to rare and serious illnesses from pathogens like herpes, influenza, hepatitis and others.
Learning and intervening
Two months after the first PMIS cases were observed, medical teams on both sides of the Atlantic are better prepared to receive it, children are recovering, and scientists are publishing their first broad descriptions of larger groups of patients.
Dr Mike Levin, whom Al Jazeera interviewed in May, has learned that children with PMIS can be broadly separated into three groups, with some at the highest risk for heart injury.
In a paper published in June, his team wrote that the illness might be provoked by the body’s own immune response, suggesting (but not yet proving) that the antibodies tuned to target the SARS-CoV-2 virus’s infamous spike protein may cause the immune system to backfire, enhancing the capacity of the virus to enter and harm cells (a surprising outcome that has been seen before in dengue fever).

Dr Ofori-Amanfo has learned how to assess risk among incoming patients, how to target specific treatments and how to follow-up to ensure their hearts remain healthy. He is from Ghana, and collaborates regularly with physicians there. Though his colleagues have not yet seen PMIS in their hospitals, Dr Ofori-Amanfo is becoming more confident that some universally available interventions could be deployed quickly should they be needed, even in developing world contexts.
David Vargas is back at home, preparing for senior year and thinking about university. College applications are expected in the autumn, and he wants to study engineering, architecture or interior design. For now, with summer sport and activities mostly cancelled because of the coronavirus, he will focus on art.
On being one of the first to have had PMIS and recovered, he says: “I don’t think about it that much, but I have thought about it. I’m one of the first cases of this mysterious syndrome.”
“To see that coronavirus did a 180 [degree turn] and is starting to get little kids and teenagers sick,” he adds, “this virus is completely unpredictable.”