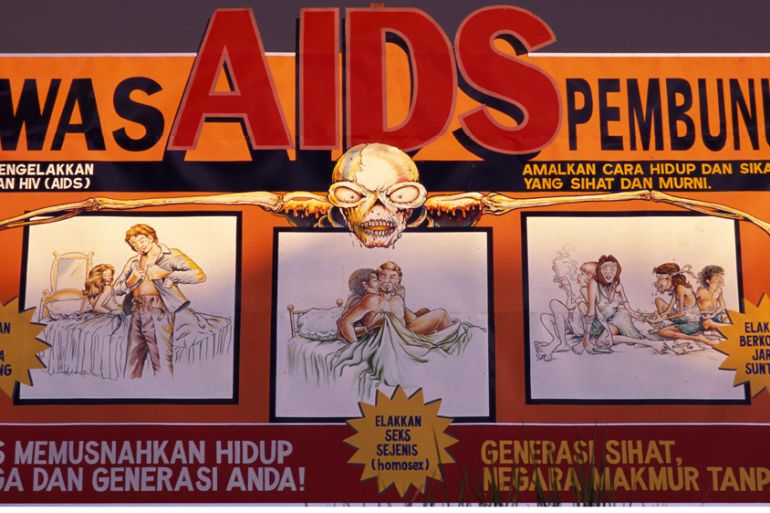
Malaysia: Halting HIV and drug use with compassion
Innovative harm-reduction scheme has dramatically reduced infection rates, but donors are suffering HIV ‘fatigue’.
Kelantan, Malaysia – Outreach workers armed with sterile needles, condoms, and screw caps patrol the narrow river that marks Malaysia’s northern border with Thailand, looking for men from both countries who gather there to take drugs.
Even though punishments for drug use in the Southeast Asian nation are severe, none of the users they meet are likely to be arrested. The police know what’s going on but stay away.
Keep reading
list of 4 itemsUS to consider visa restrictions over Uganda anti-gay law
US relaxes restrictions for gay, bisexual men to donate blood
Biden administration appeals US ruling on health coverage mandate
The workers are the front line in Malaysia’s 10-year-old harm reduction programme that has helped curb a disturbing rise in HIV infections among injecting drug users. Cooperation between health officials, civil society groups, and the police has also eased widespread scepticism about needle exchanges and the provision of methadone treatment for people addicted to drugs.
|
|
| The Battle Against HIV/AIDS Promo |
“We needed this programme, and we needed it to be quick,” said Dr Ilias Adam Yee, executive director of the Malaysian AIDS Council. “The epidemic was blowing up.”
In Kelantan, the site of the Golok River, the HIV infection rate was running at four times the national average before harm reduction was introduced.
“The reality is that we cannot stop them from getting involved in drugs, so we make sure when they do, they can use a clean syringe and have safe sex,” explained Dr Ahmad Razin Ahmad Mahir from the Ministry of Health in Kelantan.
“That is the crux of the programme. Our interest is to control HIV, and we have managed to do that.”
Yet, despite growing evidence that the programme reduces the risk of HIV and helps wean users off hard drugs, global funding for such initiatives – already only seven percent of the $2.3bn UNAIDS estimates is needed in 2015 – is under threat as donor priorities shift.
RELATED: UN: World can end AIDS epidemic by 2030
The Global Fund to Fight AIDS, Tuberculosis and Malaria – or simply, the Global Fund – is the leading international donor for harm reduction initiatives across the world, recently changed the way it funds projects to take into account each country’s income level (as calculated by the World Bank), their ability to pay, and national disease burden.
“We see funding for needle exchange-based programmes double compared with the round-based [funding] model,” said Mauro Guarinieri from the Global Fund.
“We see that there’s a focus on high-impact intervention that can really make a difference in producing a real decrease of new infections. That’s a good signal,” Guarinieri said.
But civil society groups are sceptical about the longer-term implications.
“All of this is occurring in a broader global context where what we call HIV fatigue is happening at the international donor level,” Rick Lines, executive director at Harm Reduction International, told Al Jazeera.
“It’s not the priority issue at an international level that it would have been 10 or 20 years ago. The outcome is that programmes close,” Lines explained. “If international donor support ends and national governments don’t step in, inevitably, people will go back to unsafe behaviour – sharing syringes and needles being the most obvious.”
Senior officials admit the changes mean international funding will inevitably focus on poorer places, rather than middle-income countries that are home to 75 percent of all people who inject drugs. In many of those nations, particularly in Eastern Europe and Asia, governments are unwilling to pay for harm reduction, putting long-running programmes at risk.
“We really require more of upper middle-income countries,” said Marijke Wijnroks, chief of staff at the Global Fund. “It’s not that we have all the money in the world. We have to set priorities.”
RELATED: Campaigners: ‘Beginning of the end’ for AIDS
The uncertainty surrounding harm reduction comes as the international community prepares for the first UN General Assembly Special Session (UNGASS) on drugs in 20 years – scheduled for April 2016.
Campaigners say it was the last UNGASS in 1998, which concluded with a pledge to create a “drug-free world”, that spurred the increasingly punitive approach to drugs and a crackdown that’s estimated to cost at least $100bn a year.
They say governments should start redirecting that funding to harm reduction with a goal of 10 percent by 2020.
|
|
| Saving Mary Jane |
“There are billions of dollars being spent on drug programmes. It’s not a matter of looking for new money,” Lines said.
“It’s already being spent on prisons, police, involuntary drug treatment – all kinds of things we would argue are ineffective, often counterproductive, and even abusive.
“Even a redirection of a tiny percentage of that [money] into evidence-based, harm reduction programmes would revolutionise the HIV response among people who inject drugs around the world,” Lines said.
Malaysia’s harm reduction programme is funded almost entirely by the government. The Ministry of Health says the programme reaches as many as 80 percent of the country’s estimated 170,000 injecting drug users.
New HIV infections among drug users have more than halved since 2006 and those who’ve started methadone treatment are also more likely to have found stable jobs.
In Kelantan, the authorities spend between $1.2m and $1.7m on harm reduction. HIV infections dropped to 277 last year, compared with more than 1,200 before the programme started.
RELATED: Executing drug dealers in Southeast Asia
On the banks of the Golok River, 37-year-old Mohd Azani sat sucking on a local, juicy lychee-like fruit known as mata kucing.
He started smoking heroin 15 years ago because his friends were doing it. Five years later, he was injecting, spending about $2.50 on each of his three daily hits and struggling to hold down a job.
Azani started coming to the Golok mobile clinic two years ago. Relieved that he wasn’t HIV-positive, he is now in his third month of methadone therapy.
“I want to have a good family, have children, and get my life sorted out,” he said, standing on the river bank. “I regret taking drugs. It’s just a waste of time and money.”